The future of conventional medicine.
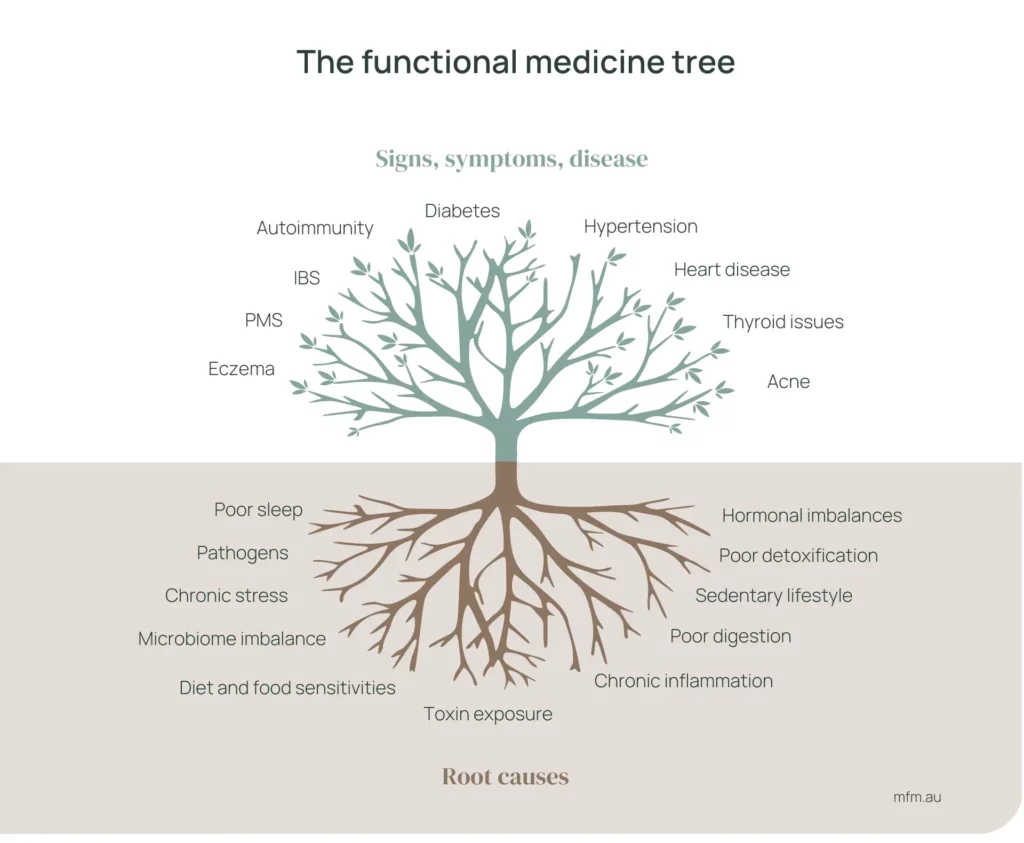
Functional Medicine is an approach to healthcare that focuses on treating the root cause of illness rather than merely addressing symptoms. It involves an in-depth understanding of a patient’s history, genetic makeup, environment, and lifestyle factors that may contribute to their health issues.
Functional medicine is the future of traditional medicine. It sees the body as a single, unified system, not just a collection of independent organs operating separately. This practical approach to medicine treats the entire system, the whole body, rather than just the symptoms.
Key principles of Functional Medicine often include:
1. Personalized Care: It emphasizes personalized treatment plans tailored to each individual’s unique biochemical makeup, genetics, and lifestyle.
2. Tests and assessment: Functional medicine practitioners provide various specialized tests aimed at uncovering underlying health issues and imbalances. Tests like Stool Tests, blood tests, breath tests, genetic testing, nutritional assessments, environmental toxin testing, comprehensive thyroid panel (TSH, T4, T3, rT3, TPOAb, TGAb and TRAb..), and more.
3. Holistic Approach: Functional Medicine considers the whole person rather than isolating symptoms or individual organs, aiming to address the interconnectedness of various bodily systems.
4. Finding the Root Cause: Instead of solely managing symptoms, Functional Medicine practitioners strive to identify and address the underlying factors contributing to health problems.
5. Integrative Treatments: It often combines conventional medicine with alternative or complementary therapies, such as nutrition, supplements, stress reduction techniques, and lifestyle modifications.
Several root causes are often considered significant contributors to various diseases in the context of Functional Medicine.
Among these, inflammation and gut dysbiosis stand out as key factors that can impact overall health and contribute to the development of numerous conditions.

– Inflammation:
Chronic inflammation is associated with a wide range of diseases, including cardiovascular diseases, diabetes, autoimmune disorders, certain cancers, and more. It’s the body’s natural response to injury or infection, but when it becomes chronic due to factors like poor diet, stress, lack of exercise, or environmental toxins, it can lead to tissue damage and various health issues.
– Gut Dysbiosis:
The gut microbiome plays a crucial role in maintaining overall health. Dysbiosis refers to an imbalance or disruption in the gut microbial community, where there’s an overgrowth of harmful bacteria (like Candida) or a decrease in beneficial bacteria. This imbalance can contribute to digestive problems, autoimmune conditions, mental health issues, allergies, and more. Factors such as diet, antibiotics, stress, and certain medications can disrupt the gut microbiota.
Other potential root causes that Functional Medicine considers include:
– Nutrient Deficiencies:
Inadequate intake or absorption of essential nutrients can impact various bodily functions and contribute to health issues.
– Toxin Exposure:
Environmental toxins from sources like pollution, pesticides, heavy metals, and certain chemicals may contribute to disease by disrupting normal bodily functions.
– Stress and Mental Health:
Chronic stress, unresolved trauma, and mental health conditions can have a profound impact on physical health, affecting hormone levels, immune function, and more.
– Genetic Predisposition:
While genetics play a role, it’s often the interplay between genes and environmental factors that determines disease susceptibility.
The diagnosis of a disease can result from more than one cause. For instance, depression can stem from various factors, such as inflammation in the body, while inflammation can similarly lead to various illnesses like depression. Conventional medicine focuses on treating diseases when they are already present rather than preventing them, primarily by suppressing the symptoms with prescription drugs, without addressing the underlying cause of the disease.
Functional medicine is a map, it’s a GPS system, a way of navigating through the landscape of an illness. It’s the medicine that connects the dots between all the things that are going wrong in our biology.
- Dr. Mark Hyman Tweet
Functional Medicine aims to identify and address these underlying root causes through personalized treatment plans that may involve dietary changes, targeted supplements, stress management techniques, lifestyle modifications, and sometimes medication or other interventions, all tailored to an individual’s specific needs and circumstances.
Medications in traditional medicine often address only the symptoms of the disease without correcting the root cause. These medications often lead to significant side effects, causing the individual to require additional medications, thus starting a cycle.

Medications can indeed be crucial and even life-saving in certain cases. However, there is a concern that doctors are prescribing an excessive number of medications, even for minor issues. Often, patients can alleviate symptoms solely through lifestyle changes, such as dietary adjustments, exercise, mindfulness practices, supplements, and more.
It’s essential to integrate both conventional medicine and functional medicine to achieve long-lasting impact and even prevent diseases.
Functional medicine practitioners run tests, like stool tests, and assessments to gain a deeper understanding of an individual’s unique health profile. This information helps them to tailor treatment plans specifically designed to address the root causes of health issues, promote overall wellness, and prevent future health problems.
Interconnectedness of the body systems is a fundamental principle in Functional Medicine.
Here are several examples illustrating how certain conditions or diseases can have various underlying causes and how different body systems are interconnected:
1. Depression and Inflammation/Gut Dysbiosis: Research suggests that chronic inflammation in the body might contribute to the development of depression. Inflammation can affect the brain and disrupt neurotransmitter function, impacting mood regulation. Additionally, imbalances in the gut microbiome (gut dysbiosis) can influence mental health. The gut-brain axis connects the gut and the brain, indicating that disturbances in gut health may contribute to mood disorders like depression.
2. Adrenal Fatigue and Stress/Toxic Overload: Adrenal fatigue, though not a recognized medical diagnosis, is often associated with chronic stress. Prolonged stress can lead to dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis, impacting the adrenal glands and causing fatigue. Furthermore, exposure to environmental toxins can burden the body’s detoxification systems, including the liver, leading to an overload that contributes to fatigue and disrupts hormonal balance.
3. Autoimmune Conditions and Gut Health/Nutrient Deficiencies: Many autoimmune diseases, such as rheumatoid arthritis and Hashimoto’s thyroiditis, have links to gut health and nutrient deficiencies. Dysbiosis in the gut can contribute to increased intestinal permeability (leaky gut), allowing substances to pass into the bloodstream and trigger immune responses, potentially leading to autoimmune reactions. Nutrient deficiencies, especially vitamin D, B vitamins, and essential minerals, can also impact immune function and contribute to autoimmune conditions.
4. Chronic Fatigue Syndrome (CFS) and Mitochondrial Dysfunction/Infections: Chronic Fatigue Syndrome is a complex condition with multifactorial origins. Some studies suggest that mitochondrial dysfunction, where cells struggle to produce energy efficiently, may play a role in CFS. Additionally, certain viral or bacterial infections (such as Epstein-Barr virus or Lyme disease) are believed to trigger or contribute to the development of CFS in susceptible individuals.
5. Skin Conditions and Gut Health/Inflammation: Skin conditions like eczema, psoriasis, and acne may have connections to gut health and inflammation. Dysbiosis in the gut can lead to systemic inflammation, which may manifest as skin issues. Moreover, imbalances in the gut microbiome can impact the immune system, influencing inflammatory responses that manifest on the skin.
6. Insulin Resistance and Inflammation/Lifestyle Factors: Insulin resistance, a precursor to type 2 diabetes, is influenced by inflammation and lifestyle factors. Chronic inflammation can impair insulin signaling, leading to insulin resistance. Lifestyle factors such as poor diet, lack of exercise, and stress contribute to inflammation and insulin resistance.
These examples highlight the intricate connections between various body systems and how disturbances in one area can impact seemingly unrelated functions or organs. Functional Medicine aims to identify and address these interconnected root causes to provide more comprehensive and personalized approaches to healthcare.
In conclusion:
Functional Medicine represents a paradigm shift in healthcare, focusing on personalized, comprehensive approaches that aim to uncover and address the root causes of illness. Unlike traditional medicine, which often focuses on managing symptoms through medications, Functional Medicine delves deeper into an individual’s unique genetic, environmental, and lifestyle factors to develop personalized treatment plans.